Navigating Ethical Dilemmas: A Nurse’s Guide To Reporting Suspected Maltreatment
(1) Licensed medical professionals, emergency services personnel, facility employees, skilled nursing facility employees, employees of an entity responsible for providing care to a vulnerable adult, medical examiners, social workers, or law enforcement personnel
who have reasonable cause to believe that a vulnerable adult is being or has been maltreated shall report such information to the commission’s designated APS provider as expeditiously as possible but within twenty-four (24) hours of acquiring the information that forms the basis of such reasonable cause.
When there is reasonable cause to believe that maltreatment has resulted in death or serious physical injury jeopardizing the life, health, or safety of a vulnerable adult, any person required to report under this section shall also report such information as expeditiously as possible to the appropriate law enforcement agency but within four (4) hours of acquiring the information that forms the basis of such reasonable cause. Ombudsmen recognized by the commission are exempt from reporting maltreatment that is discovered in the course of their duties.
(2) Failure to report as provided under this section is a misdemeanor subject to punishment as provided in section 18-113, Idaho Code.
(3) Any person, including any officer or employee of a financial institution, who has reasonable cause to believe that a vulnerable adult is being abused, neglected, or exploited may report such information to the commission or its providers.
TITLE 39 HEALTH AND SAFETY CHAPTER 53 ADULT ABUSE, NEGLECT AND EXPLOITATION ACT. 39-5303. DUTY TO REPORT CASES OF VULNERABLE ADULT MALTREATMENT
- Navigating Ethical Dilemmas: A Nurse’s Guide To Reporting Suspected Maltreatment
- In Idaho, Healthcare Professionals Are Indeed Legally Obligated To Report Certain Types Of Incidents, Including The Abuse, Neglect, Or Exploitation Of Vulnerable Adults.
- What Exactly Does Janette’s Text Mean?
- If A Person Is Terminally Ill And Their Doctor Estimates They Have Six Months To Live, But A Registered Nurse (Who Is Also Your Sister) Convinces The Family That The Doctor’s Prognosis Is Incorrect And Accuses The Hospice Of Allowing Excessive Administration Of Narcotics To The Patient, What Civil Torts Or Criminal Laws Could The Nurse Be Violating?
- Is It Ever Too Late To Report A Potential Violation Of Professional Ethical Standards For A Registered Nurse, If Not, Who Do You Report It To?
- Is Foul Play An Actual Legal Concept?
- Did The Hospice Nurse Report Janette To The Doctor In Charge?
- Janette Says: “I’m So Sad That No One Sees How Wrong This Is.”
- Was Janette Defaming Denise When Janette Voiced Her Opinion (Lied) Claiming Andrea Is Not Dying?
- Are Registered Nurses Licensed Medical Professionals?
- Does Janette Have Reasonable Cause To Believe That Andrea Was Being Maltreated That Resulted In Death?
- Why Did Janette Refuse To Report Denise To APS Or Law Enforcement?
- Did Janette Actually Report Denise To Anyone If Janette Honestly Believes Denise And/Or Hospice Is Helping Andrea Die?
- What Is Ejection Fraction?
- What Is The Life Expectancy Of A Patient With An Ejection Fraction Of 25% Or Less?
- Does Janette Have A Pattern Of Behavior For Contradicting Doctors And/Or Hospice Services?
- Are Registered Nurses Required By Law In Idaho To Have Malpractice Insurance?
- Do Nurses Typically Have Malpractice Insurance?
- Could Janette Be Subject To Criminal Penalties For Refusing To Report Her ‘Belief’ That Denise, Hospice, And/Or Andrea’s Doctors Were Assisting Andrea In Speeding Up Andrea’s Death?
- In Idaho, If A Healthcare Professional Believes A Family Member Is Attempting To Use Hospice To Assist Their Daughter In Speeding Up Their Death, Is The Licensed Healthcare Worker Required — By Law — To Report This Matter To The Police Or At Least To Her Supervisor?
- Is It Legal For A Registered Nurse To Contradict The Doctor’s Order To The Patient?
- If A Registered Nurse Or Family Member Is Fully Convinced That Their Sister Is Accelerating The Death Of Her Daughter In Hospice Care And Chooses Not To Report This To The Authorities, Could They Be Held Legally Responsible If The Court Later Finds That This Action Constituted Maltreatment Leading To Death?
In Idaho, Healthcare Professionals Are Indeed Legally Obligated To Report Certain Types Of Incidents, Including The Abuse, Neglect, Or Exploitation Of Vulnerable Adults.
According to Idaho Code § 39-5303, licensed medical professionals, among others, who have reasonable cause to believe that a vulnerable adult is being or has been maltreated must report such information to the appropriate Adult Protective Services (APS) provider.
This reporting should be done as soon as possible but within twenty-four hours of acquiring the information that forms the basis of such reasonable cause.
Furthermore, if there is reasonable cause to believe that such maltreatment has resulted in death or serious physical injury jeopardizing the life, health, or safety of a vulnerable adult, the incident must also be reported to the appropriate law enforcement agency within four hours of acquiring the information.
- It’s important to note that failure to report as required under this section is considered a misdemeanor.
Additionally, those who make reports in good faith are immune from liability, while those who report falsely or in bad faith may face actual damages or statutory penalties.
Therefore, if a healthcare professional in Idaho suspects that a family member is using hospice care to hasten the death of a patient, they would be required by law to report this to the appropriate authorities, which could include Adult Protective Services or law enforcement, depending on the severity of the situation.
This obligation is in line with the overarching principle to ensure the safety and well-being of vulnerable individuals in care settings.
For more detailed information, you can refer to the Idaho State Legislature website.
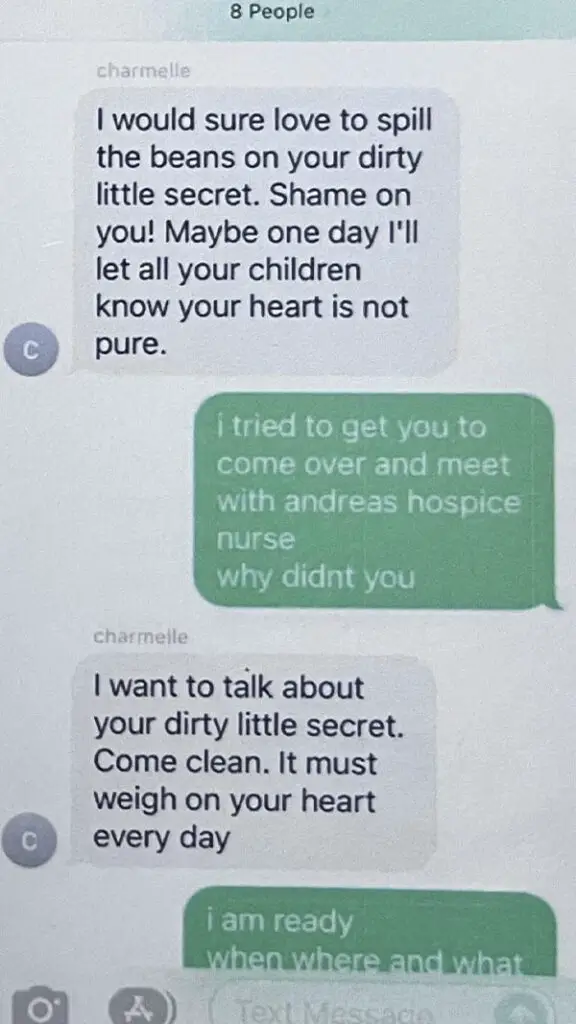
What Exactly Does Janette’s Text Mean?
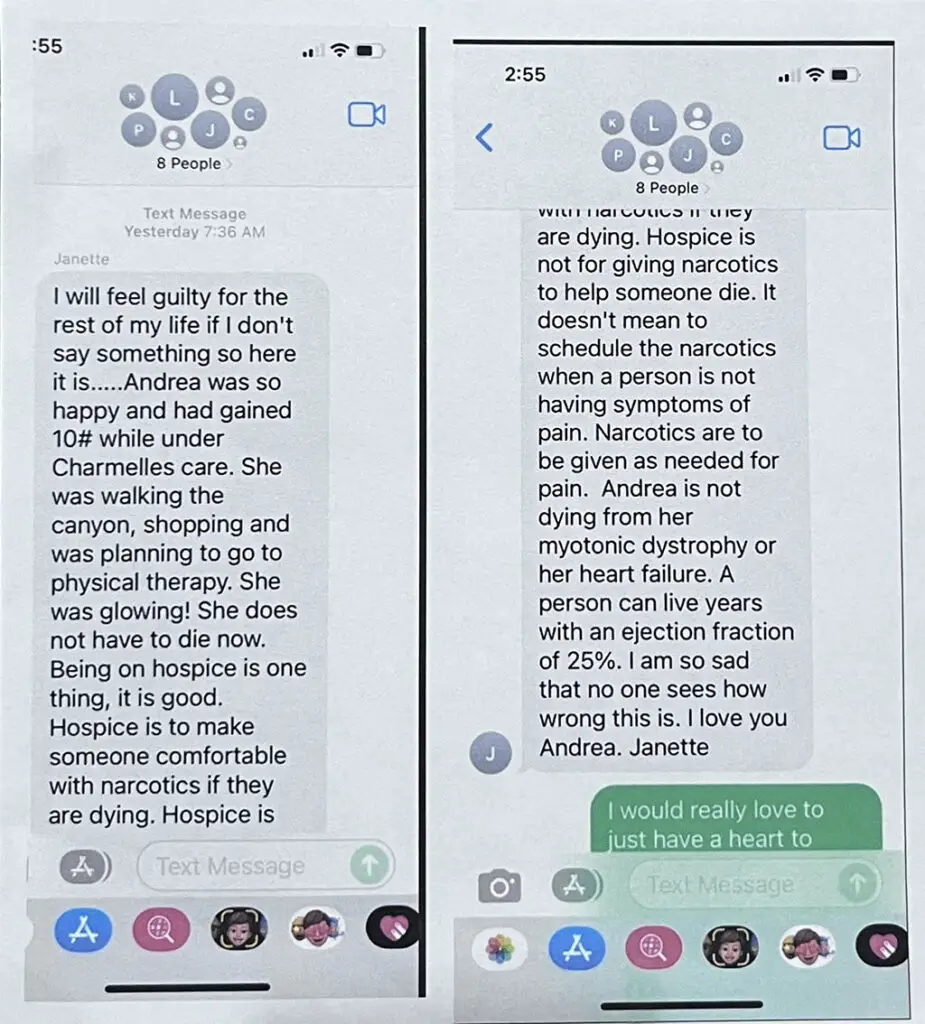
Janette expresses deep concern and guilt about the situation with Andrea, who was under Charmelle’s care and showed significant improvement in health and well-being.
Despite being on hospice, Andrea gained weight, was active, and appeared happy, leading Janette to believe that Andrea was not at a stage where end-of-life care was necessary.
Janette argues that hospice care should be about comfort, not hastening death, and is troubled by the use of narcotics when Andrea is not in pain.
She believes Andrea’s condition (myotonic dystrophy and heart failure with an ejection fraction of 25%) is not immediately life-threatening and feels saddened by what she perceives as a wrongful approach to Andrea’s care.
Janette’s statement reflects a mix of love, sadness, and a sense of moral obligation to speak out.
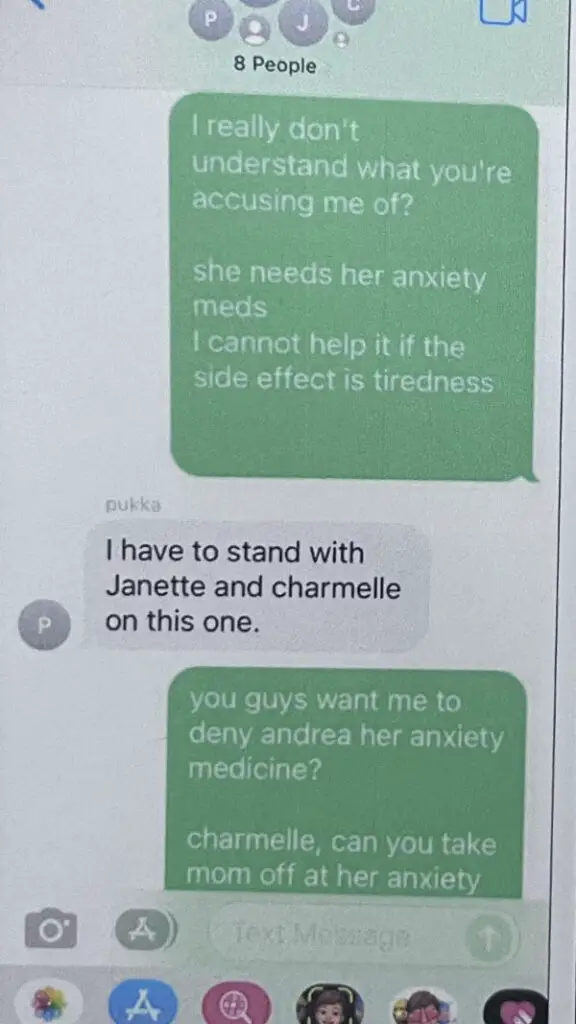
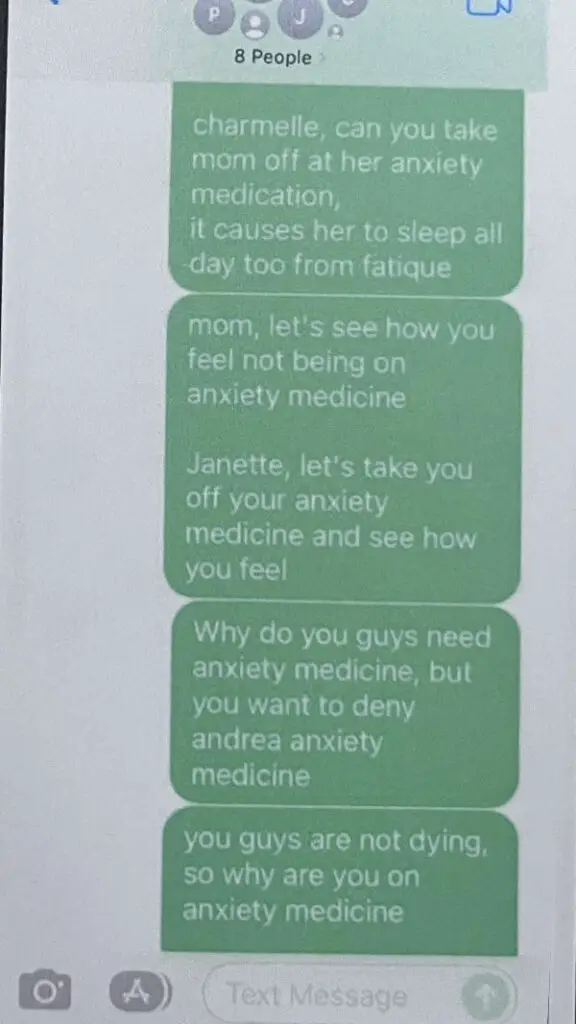
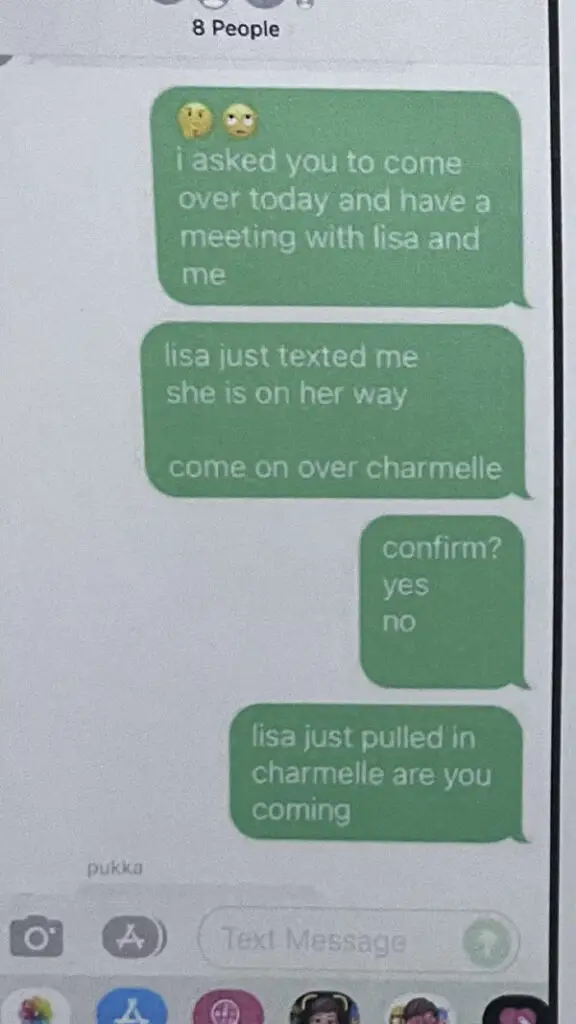
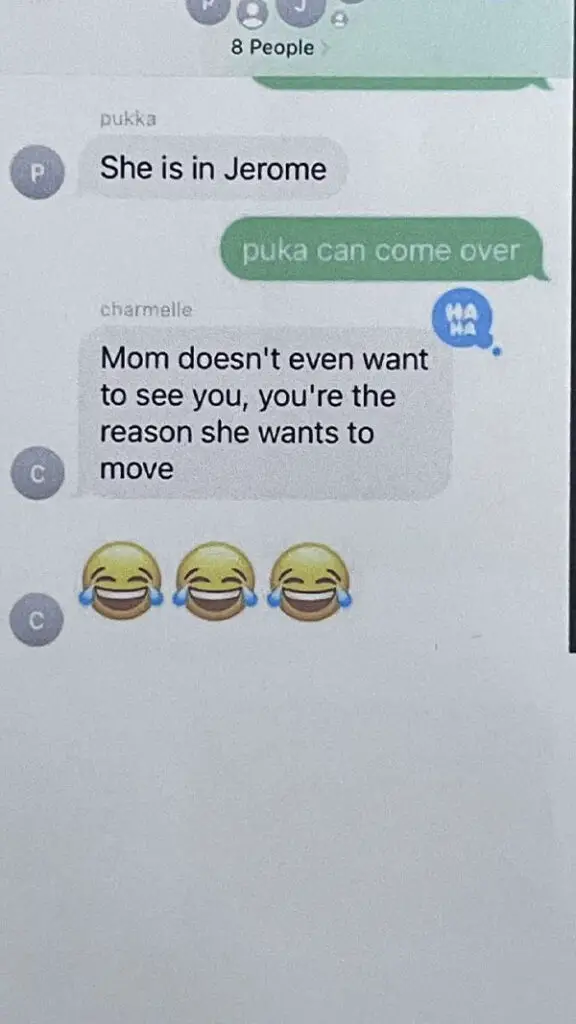
Denise’s Responds To Janette’s Group Text
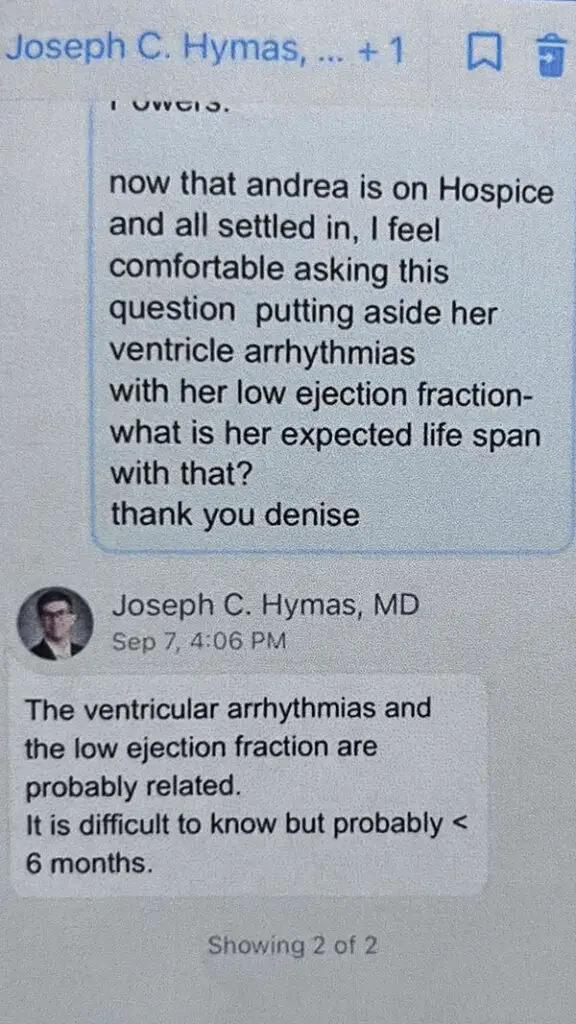
Even though Andrea’s doctor says Andrea’s life expectancy is less than six (month), Janette, Charmelle, and Marjorie believe otherwise.
Who do you listen to?
Your nurse sister or the medical doctor?
Maybe Janette, Charmelle, and Marjorie did report Denise to law enforcement?
Did law enforcement find their claim to not meet the criminal standards of BEYOND A REASONABLE DOUBT?
What Reasonable Doubt Is There To Suggest Denise Did Not Kill Andrea Or Assist Andrea In Dying Faster — As Janette, Charmelle, And Marjorie Claim?
- Andrea’s doctor said Andrea probably has less than six months.
- According to the Journal of Palliative Medicine, about 90% of patients die within the six-month timeframe after entering hospice. If a patient has been in hospice for six months but a doctor believes they are unlikely to live another six months, they may renew their stay in hospice.
- Andrea went on hospice on or about September 1, 2022 and passed away on December 7, 2022. That’s 3 months, 6 days excluding the end date or 97 days.
Click image below to open gallery
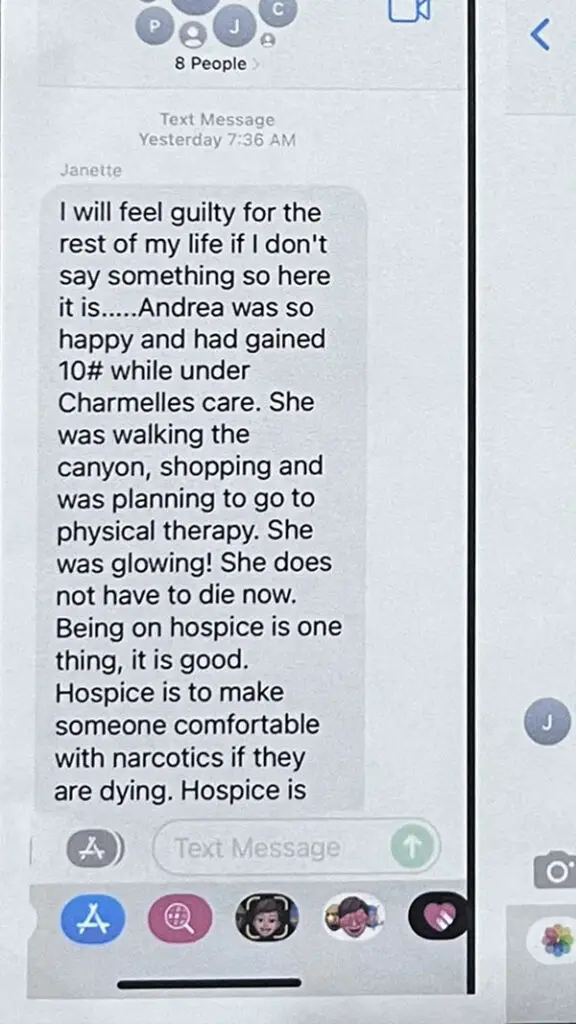
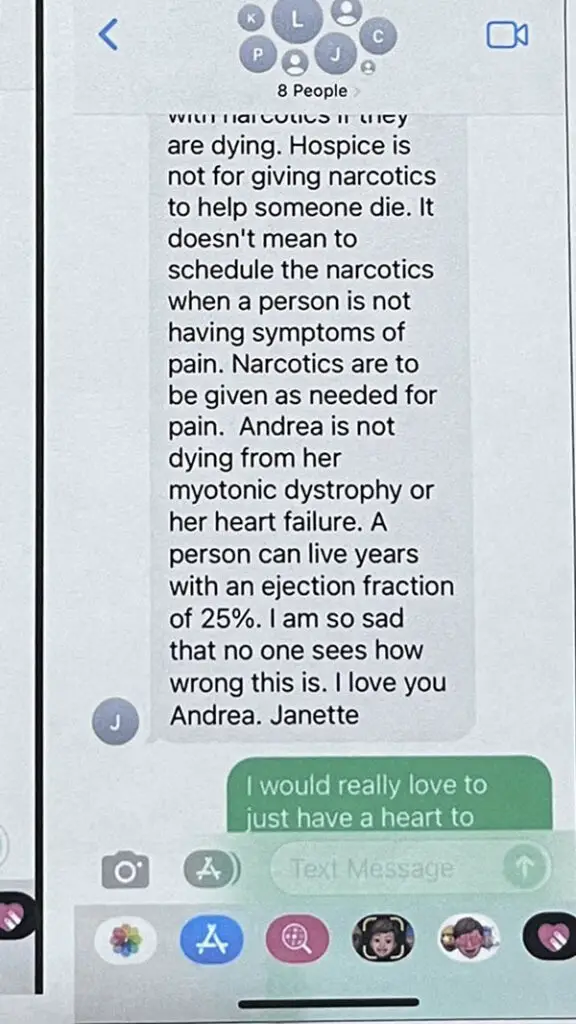
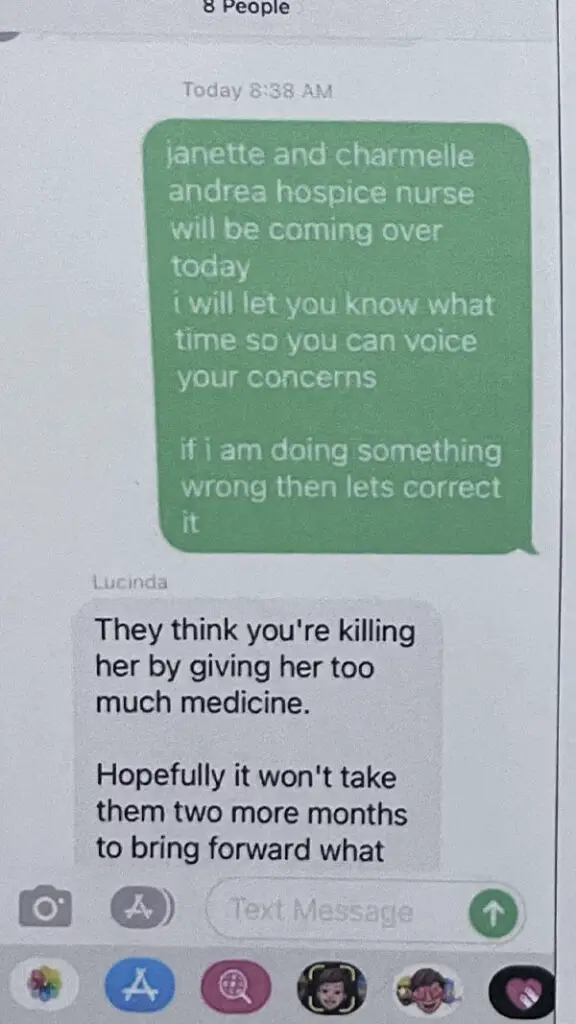
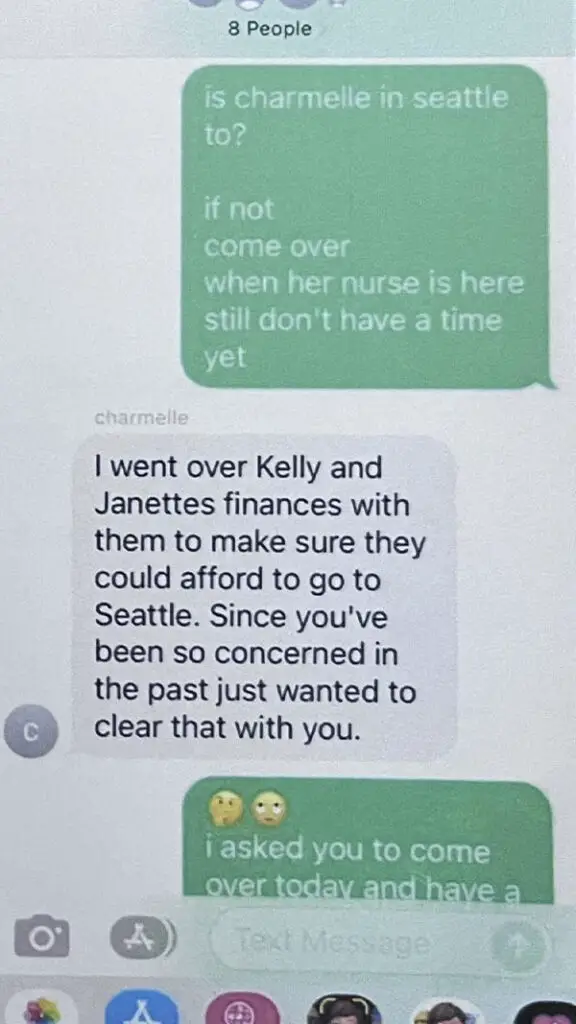
Janette, in a group email, expressed concerns that Andrea’s hospice team were improperly administering narcotics.
When Andrea’s hospice nurse learned of Janette’s claims, she mentioned their malpractice insurance and informed the prescribing doctor about Janette’s accusations.
The nurse noted that the doctor was aware of Janette and held a negative opinion of her.
This suggests that Janette’s allegations were viewed as unjustified and potentially damaging to the hospice’s reputation.
Janette has raised concerns about Horizon Home Health and Hospice, suggesting foul play regarding medication administration.
When Andrea’s hospice nurse was informed of this, she mentioned the hospice’s malpractice insurance.
The nurse later informed the prescribing doctor about Janette’s claims, revealing the doctor’s unfavorable view of Janette.
These actions indicate that Janette’s accusations were taken seriously, though viewed negatively.
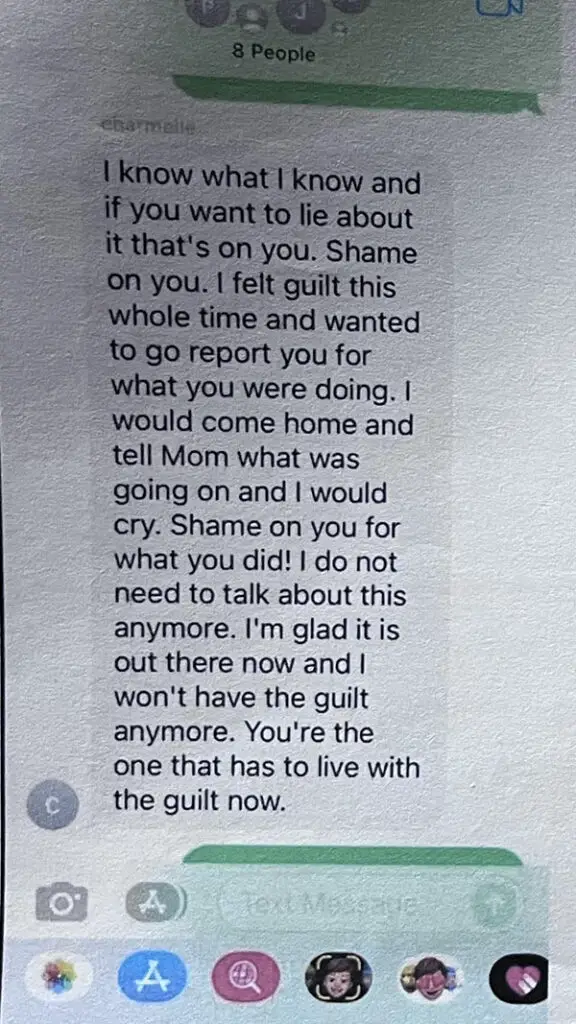
Additionally, Charmelle’s email supports Janette’s claims, highlighting that another hospice nurse also made allegations against the hospice company.
The issue revolves around the use of morphine and Ativan for end-of-life comfort, not to hasten death.
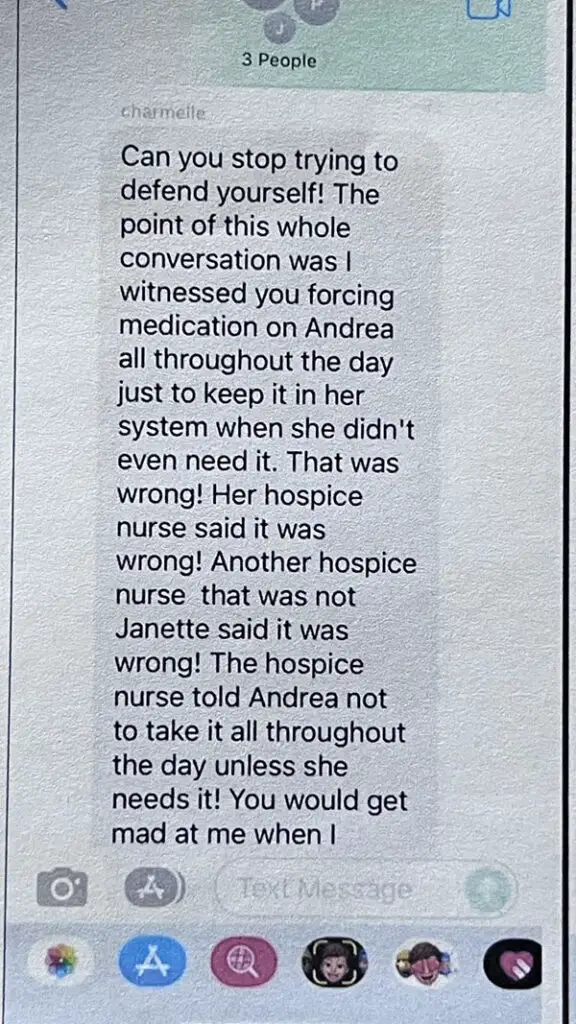
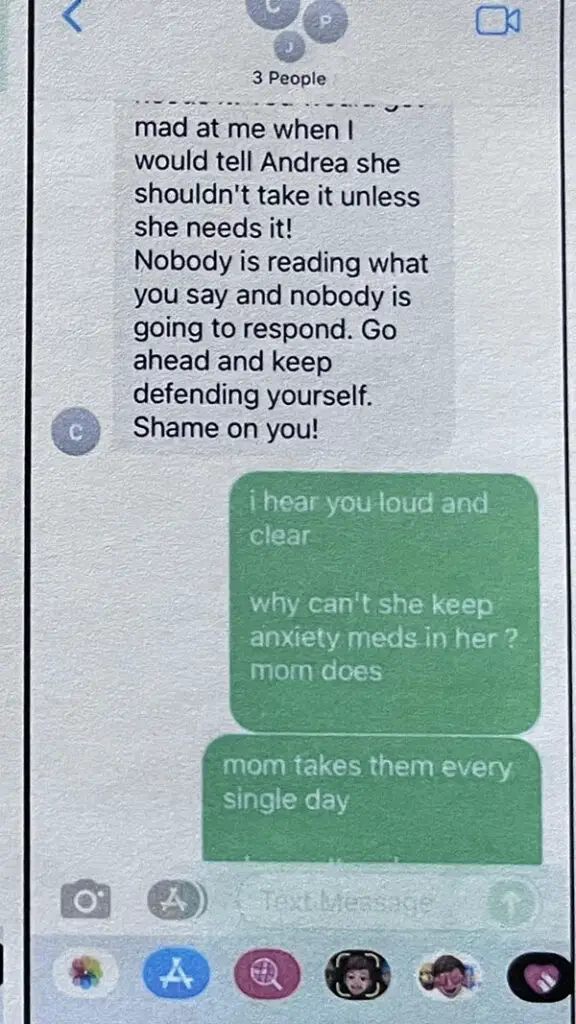
- Denise was giving Andrea Ativan.
- 3x a day to help with excessive nighttime anxiety.
- Andrea narcotic, hydrocodone as she was allergic to morphine.
- Andrea would take that as needed for air, hunger, shortness of breath.
- Andrea’s nurse advised her to take hydrocodone when she felt short of breath, because short of breath makes her scared, causing anxiety, so we had to keep it under control.
- Charmelle did not like this because it made Andrea tired and
- Charmelle wanted Andrea fully awake and happy and bubbly before she knew she was dying so it was all self-centered on her.
If A Person Is Terminally Ill And Their Doctor Estimates They Have Six Months To Live, But A Registered Nurse (Who Is Also Your Sister) Convinces The Family That The Doctor’s Prognosis Is Incorrect And Accuses The Hospice Of Allowing Excessive Administration Of Narcotics To The Patient, What Civil Torts Or Criminal Laws Could The Nurse Be Violating?
When a registered nurse, who is also a family member, disputes a doctor’s prognosis and accuses a hospice of giving excessive narcotics to a patient, several potential legal issues can arise.
The specific civil torts or criminal laws that might be violated depend on the jurisdiction, the exact nature of the actions and statements, and the outcomes of those actions.
Here are some possibilities:
- Defamation (Libel or Slander): If the nurse makes false statements about the doctor or hospice care that harm their reputations, it could be considered defamation. Slander refers to spoken defamation, while libel refers to written or published defamation.
- Interference with Professional Relationships: If the nurse’s actions disrupt the professional relationships between the patient, the doctor, and the hospice care, it could be seen as interference with contractual or business relationships.
- Practicing Medicine Without a License: If the nurse goes beyond offering advice and attempts to make medical decisions or give treatments for which she is not licensed or authorized, it could be considered practicing medicine without a license.
- Negligent or Reckless Advice: If the nurse’s advice leads to harm because it was negligent or reckless, there could be a case for negligence or even criminal recklessness, depending on the severity and the outcomes.
- Breach of Professional Duty or Ethics: While not necessarily a civil tort or criminal law violation, the nurse could be violating professional ethical standards, which could result in disciplinary action by the nursing board.
- Criminal Charges (in extreme cases): If the nurse’s actions directly lead to harm, such as convincing the family to stop necessary medical treatment, and this results in serious harm or death, criminal charges could potentially be considered.
It’s important to note that these potential violations heavily depend on the specific details of the situation, including the nurse’s actions, the statements made, the jurisdiction’s laws, and the outcomes of these actions.
Each case would need to be evaluated individually by a legal professional to determine if any laws or professional standards have been violated.
Is It Ever Too Late To Report A Potential Violation Of Professional Ethical Standards For A Registered Nurse, If Not, Who Do You Report It To?
Reporting a potential violation of professional ethical standards for a registered nurse can typically be done at any time, though the effectiveness and outcome of the report may depend on various factors.
It’s important to consider the following aspects:
- Timing and Statute of Limitations: While there’s generally no strict deadline for reporting ethical violations, some cases may be bound by a statute of limitations, particularly if they involve legal or criminal issues. However, for ethical violations, many nursing boards will consider reports even if some time has passed, especially if the violation poses ongoing risks to patient safety or professional integrity.
- Severity of the Violation: Serious violations, especially those affecting patient safety or involving illegal activities, are typically of high concern regardless of when they occurred. Nursing boards are particularly vigilant about these issues due to the potential impact on public health and safety.
- Availability of Evidence: Over time, evidence may become less accessible or reliable, which can affect the investigation process. Prompt reporting is generally more effective.
Where to Report:
- State Nursing Board or Regulatory Body: The primary entity for reporting ethical violations by a registered nurse is the state nursing board or similar regulatory agency in the country or region where the nurse is licensed. These boards have the authority to investigate complaints and impose disciplinary actions if needed.
- Employer or Healthcare Institution: If the nurse is employed by a healthcare institution, hospital, or other organization, it can be appropriate to report the violation to their supervisor, human resources department, or internal ethics committee. Many organizations have protocols for handling such reports.
- Legal Authorities: For violations that may also constitute criminal behavior (such as patient abuse or diversion of narcotics), it’s appropriate to report these to the police or other legal authorities.
Before making a report, it’s advisable to gather relevant information, such as details of the incident, dates, and any evidence you may have.
This will assist the regulatory body or employer in conducting a thorough investigation. Additionally, consider reviewing the procedures for filing a complaint with the specific nursing board or organization, as these can vary.
Remember, reporting ethical violations is an important step in maintaining professional standards in nursing and ensuring patient safety and quality of care.
Is Foul Play An Actual Legal Concept?
“Foul play” is not a specific legal term but rather a colloquial expression used to refer to dishonest or wrongful behavior, especially in the context of sports or games.
In a legal context, actions that might be described as “foul play” could involve various legal concepts such as fraud, misconduct, criminal activity, or unethical behavior, depending on the specific circumstances.
Legal terminology and definitions would vary depending on the nature of the alleged misconduct or wrongdoing.
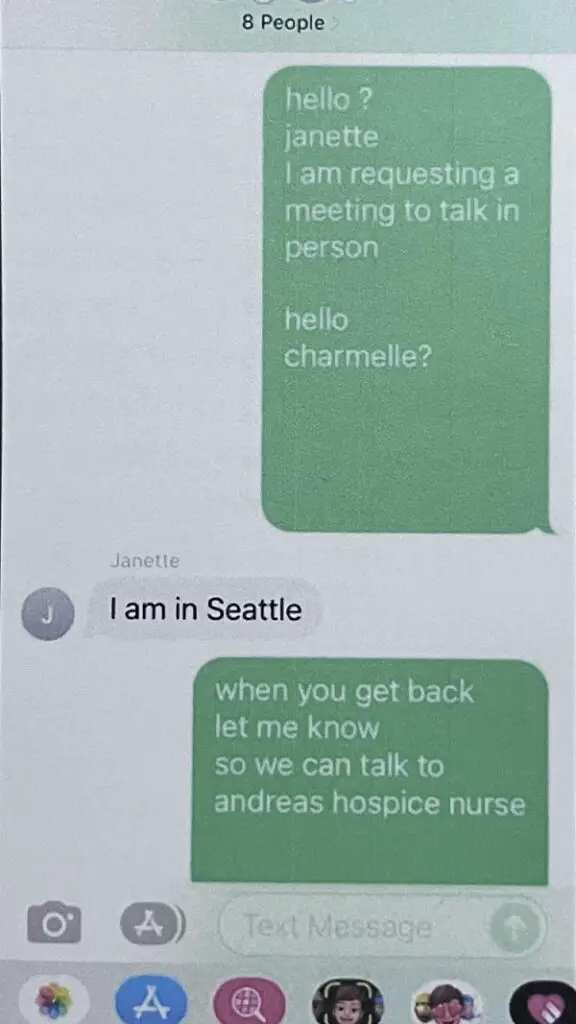
Did The Hospice Nurse Report Janette To The Doctor In Charge?
Yes, the hospice nurse reported Janette’s concerns to the doctor responsible for prescribing Andrea’s medication.
The nurse mentioned that the doctor was already familiar with Janette and did not have a favorable opinion of her.
This action suggests that the nurse took Janette’s claims seriously enough to discuss them with the doctor, despite the perceived negative view of Janette.
Janette Says: “I’m So Sad That No One Sees How Wrong This Is.”
The phrase “I’m so sad that no one sees how wrong this is” expresses deep disappointment and sadness about a situation that the speaker believes is morally or ethically wrong.
The speaker feels that others are not recognizing or acknowledging the wrongness of the situation, which adds to their distress.
It conveys a sense of frustration and isolation in their understanding or perspective of what is happening.
Was Janette Defaming Denise When Janette Voiced Her Opinion (Lied) Claiming Andrea Is Not Dying?
Determining whether Janette’s statement about Andrea — claiming that she is not dying — constitutes defamation against Denise involves several legal considerations.
Here’s a breakdown of the factors involved in determining defamation:
- Definition of Defamation: Defamation is a false statement presented as a fact that causes injury or damage to the character of the person it is about. The statement must be communicated to others, and it must be shown that the person making the statement did so negligently or maliciously.
- Truth or Opinion: For a statement to be considered defamatory, it generally needs to be a false statement of fact. If Janette’s statement is true (i.e., Andrea is indeed not dying), it cannot be defamatory. If the statement is an opinion rather than a fact, it often does not constitute defamation.
- Context of the Statement: The context in which Janette made the statement can be critical. For instance, if it was made in a private conversation versus a public forum, the implications might differ.
- Link to Denise’s Character or Reputation: To be defamatory towards Denise, Janette’s statement about Andrea would need to negatively impact Denise’s character or reputation. If Denise’s reputation or character is not affected by the statement, it might not be considered defamatory towards her.
- Harm Caused: There must be some form of harm caused by the statement. This could be damage to reputation, financial loss, or other types of harm.
- Jurisdictional Differences: Laws regarding defamation vary widely by country and even within regions of the same country. Some jurisdictions require proof of actual harm, while others consider certain statements to be defamatory per se (inherently harmful).
- Public Figures vs. Private Individuals: If Denise is a public figure, the standards for proving defamation might be higher compared to if she is a private individual.
Whether Janette’s statement that “Andrea is not dying” is defamatory towards Denise depends on the truth of the statement, the context in which it was made, its impact on Denise’s character or reputation, and the specific legal standards of the jurisdiction.
If Denise believes she has been defamed, she should consult with a legal professional who can provide advice based on the specific details and the applicable law.
Are Registered Nurses Licensed Medical Professionals?
Yes, a registered nurse (RN) is considered a licensed medical professional.
RNs are required to complete a rigorous educational program and pass a licensing examination to practice nursing.
Their license signifies that they have met the necessary criteria to provide medical care and make informed decisions regarding patient health within their scope of practice.
Being licensed also means they are accountable to standards set by the nursing regulatory body in their jurisdiction.
Does Janette Have Reasonable Cause To Believe That Andrea Was Being Maltreated That Resulted In Death?
Whether Janette has reasonable cause to believe that Andrea was being maltreated, resulting in her death, depends on the specific details and evidence available to her.
“Reasonable cause” is usually based on objective evidence or facts that would lead a prudent person to believe in the likelihood of maltreatment.
Without concrete information about what Janette observed, knew, or inferred from her interactions or observations, it’s not possible to conclusively determine if she had reasonable cause.
Why Did Janette Refuse To Report Denise To APS Or Law Enforcement?
Without specific details or context about Janette’s situation, it’s not possible to determine why she refused to report Denise to Adult Protective Services (APS) or law enforcement.
There could be a variety of reasons for her decision, ranging from personal beliefs, relationships, uncertainties about the situation, fear of repercussions, or a lack of understanding of her legal obligations.
Each scenario can have different motivations and reasoning.
To come to an accurate conclusion, more context about Janette’s circumstances and her reasoning is needed.
Did Janette Actually Report Denise To Anyone If Janette Honestly Believes Denise And/Or Hospice Is Helping Andrea Die?
Based on the information available, it’s unclear whether Janette reported Denise or anyone involved in hospice care for allegedly helping Andrea die.
If Janette, as a healthcare professional or family member, honestly believes that there is maltreatment leading to Andrea’s premature death, she would be ethically and possibly legally obligated to report it.
What Is Ejection Fraction?
Ejection fraction (EF) is a measurement used to describe the percentage of blood leaving your heart each time it contracts.
It is typically used to assess the functioning of the left ventricle, which is the heart’s main pumping chamber.
A normal EF is typically between 55% and 70%, indicating that the heart is pumping well and effectively circulating blood.
Lower EF percentages can indicate heart issues like heart failure, while very high EF values can suggest other heart conditions.
This measurement is an important tool in diagnosing and monitoring heart health.
What Is The Life Expectancy Of A Patient With An Ejection Fraction Of 25% Or Less?
Patients with an ejection fraction of 20% have a significantly reduced life expectancy.
A study cited on ScarySymptoms.com found that, among patients with ejection fractions of 20% or less, the mortality rate was 74% after three years.
However, ejection fraction alone was not a definitive predictor of survival once it dropped below or equal to 20%.
The study also noted that peak VO2, a measure of maximal oxygen consumption during exercise, was a strong predictor of mortality in these cases.
Survival rates can vary significantly depending on individual conditions and comorbidities.
For more detailed information, you can visit ScarySymptoms.com.
Does Janette Have A Pattern Of Behavior For Contradicting Doctors And/Or Hospice Services?
To be discovered to potentially establish character evidence.
Without specific information about Janette’s past actions or behavior, it’s impossible to determine if she has a pattern of contradicting doctors or hospice services.
Patterns of behavior are established through repeated, documented instances over time.
To assess whether Janette has such a pattern, one would need detailed information about her historical interactions and decisions in professional settings.
This information is typically not publicly available unless disclosed in a professional review, legal case, or similar records.
Are Registered Nurses Required By Law In Idaho To Have Malpractice Insurance?
Registered nurses in Idaho are not legally required to carry medical malpractice insurance.
Although there is no state mandate for such insurance, many healthcare facilities and insurance plans may require physicians and nurses to have malpractice insurance to practice or participate in coverage.
It’s important for medical professionals to consider obtaining coverage to protect their personal assets and professional reputation, even if it’s not a legal requirement in Idaho.
Do Nurses Typically Have Malpractice Insurance?
Yes, many nurses typically have malpractice insurance. It’s not universally mandated, but it is common practice.
This insurance provides protection against legal claims alleging negligence or errors in patient care.
While employers often provide some coverage, many nurses choose to have their own policy for additional protection, especially if they work in multiple settings or have an advanced practice role.
The decision to carry personal malpractice insurance varies based on individual circumstances and workplace coverage.
Could Janette Be Subject To Criminal Penalties For Refusing To Report Her ‘Belief’ That Denise, Hospice, And/Or Andrea’s Doctors Were Assisting Andrea In Speeding Up Andrea’s Death?
Janette could potentially face criminal penalties for failing to report her belief that Denise, hospice, or Andrea’s doctors were assisting in speeding up Andrea’s death.
In many jurisdictions, healthcare professionals are mandated reporters for suspected abuse or neglect, which may include actions leading to a patient’s premature death.
If the law categorizes her failure to report as a violation, she could be liable.
The specifics would depend on the local laws and the details of the case.
Legal consequences usually arise when there’s a clear mandate to report and a failure to do so.
In Idaho, If A Healthcare Professional Believes A Family Member Is Attempting To Use Hospice To Assist Their Daughter In Speeding Up Their Death, Is The Licensed Healthcare Worker Required — By Law — To Report This Matter To The Police Or At Least To Her Supervisor?
In Idaho, as in many other jurisdictions, healthcare professionals have specific legal and ethical obligations, particularly when it comes to patient safety and welfare.
If a healthcare professional believes that a family member is attempting to use hospice care to hasten a patient’s death, there are certain steps they are generally required to take:
- Reporting to Supervisors or Authorities: Healthcare professionals are typically required to report any suspicions of abuse or neglect, including situations where someone might be attempting to hasten a patient’s death, to their supervisor or appropriate authorities. This could be a hospital or hospice administration, an ethics committee, or a regulatory body.
- Confidentiality and Professionalism: Healthcare professionals must maintain patient confidentiality. Discussing a patient’s health or personal matters with unauthorized individuals, including other family members not involved in the patient’s care, could be considered a breach of confidentiality.
- Mandatory Reporting Laws: In many places, including Idaho, there are mandatory reporting laws that require healthcare professionals to report suspected abuse or neglect of vulnerable individuals, which can include patients in hospice care. The specifics of these laws can dictate whom the professional should report to and under what circumstances.
- Involvement of Law Enforcement: If the situation is believed to involve criminal activity, such as assisted suicide or euthanasia (if illegal in the jurisdiction), law enforcement may need to be involved. However, this is usually done after internal reporting and consultation with supervisors or legal advisors.
- Ethical Considerations: Apart from legal obligations, healthcare professionals also have ethical duties to protect their patients and to act in their best interests. This ethical duty guides their actions in complex situations like the one described.
It’s important to note that the exact legal requirements can vary based on the state and the specific circumstances of the case.
In Idaho, healthcare professionals should be familiar with state-specific laws and regulations regarding reporting suspected abuse or neglect, as well as laws relating to end-of-life care.
In Idaho, a healthcare professional suspecting that hospice care is being misused to hasten a patient’s death should report their concerns through appropriate channels, which typically include supervisors or regulatory bodies, rather than discussing the matter with multiple family members.
If there are doubts about the correct course of action, consulting with legal advisors or ethics committees is advisable.
Is It Legal For A Registered Nurse To Contradict The Doctor’s Order To The Patient?
Nurses are not always required to follow a doctor’s order if they believe it compromises patient safety or conflicts with personal or religious beliefs.
However, they cannot arbitrarily choose which orders to follow. If a nurse has safety concerns, especially regarding medication or procedures that conflict with facility policies, they should consult a peer or charge nurse and notify their supervisor.
Declining to follow orders due to personal or religious beliefs should also be reported to managers or supervisors.
Nurses have a responsibility to inform a supervisor and the physician immediately to prevent delays in patient care, and failure to do so may constitute negligence.
They might face disciplinary actions by their employer and the board of nursing if proper steps are not followed.
For more detailed information, you can refer to the Registered Nursing website.
If A Registered Nurse Or Family Member Is Fully Convinced That Their Sister Is Accelerating The Death Of Her Daughter In Hospice Care And Chooses Not To Report This To The Authorities, Could They Be Held Legally Responsible If The Court Later Finds That This Action Constituted Maltreatment Leading To Death?
As a registered nurse or family member, if you consciously choose not to report a belief of maltreatment in a hospice setting that leads to a death, you could potentially face legal consequences.
The degree of liability would depend on various factors, including your role, the specific circumstances, and applicable laws.
Healthcare professionals, in particular, have a legal and ethical obligation to report suspected maltreatment.
Failure to do so could be viewed as neglect or complicity, especially if there is a legal mandate to report such suspicions.
However, determining legal liability would ultimately depend on the findings of a court of law or relevant regulatory bodies.